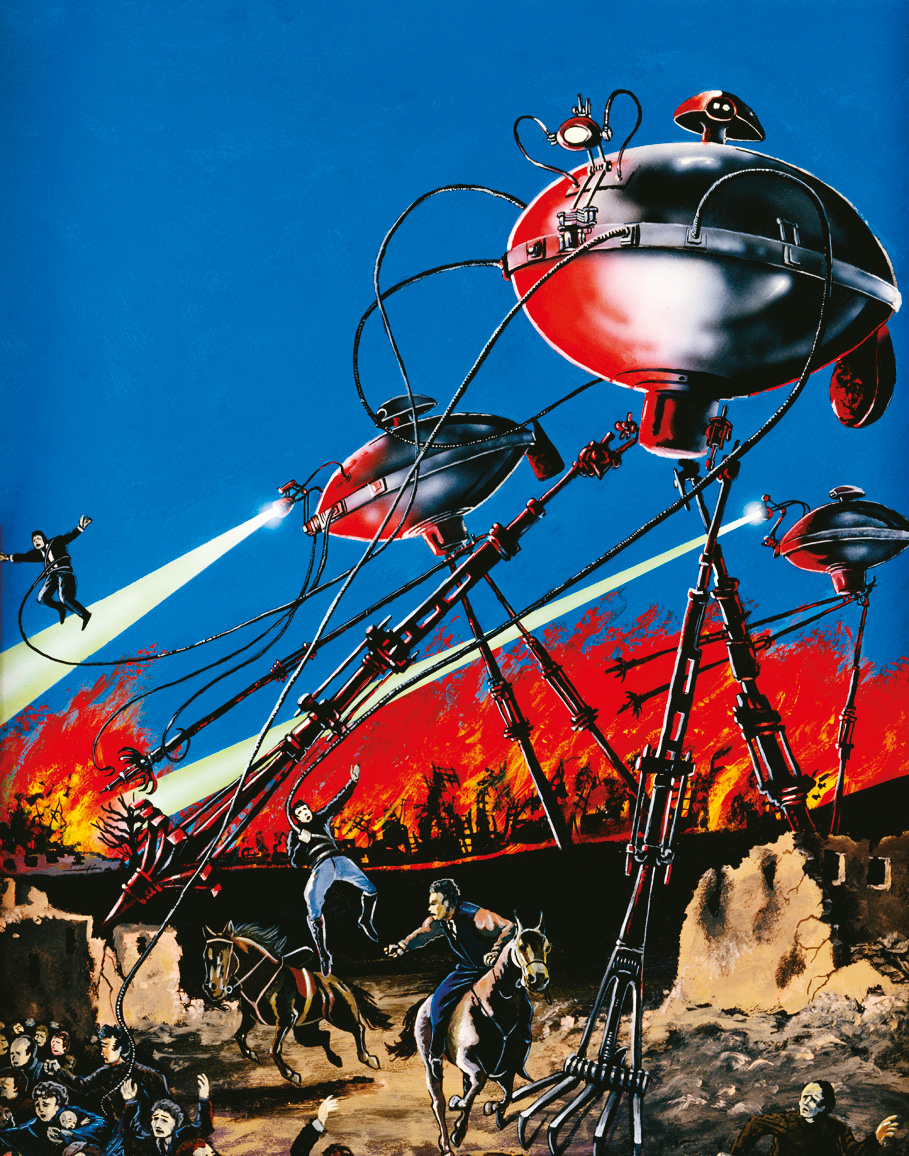
Deadly cargo
Minute and lethal, the virus that caused the 1918 Spanish flu killed more than 50 million people in a matter of months. Now it is evolving into new, highly infectious strains—including swine flu—that have scientists fighting to contain them.
When the Union Steam Ship Company’s liner Niagara tied up at Auckland’s Queen’s Wharf on a brisk October morning in 1918, a lethal cargo came ashore with the steamer’s passengers: influenza.
Within weeks, the country was in the grip of the most catastrophic pandemic in its history, one that in the course of just a few weeks would test its emergency services to the limit and leave 8600 people dead—almost half the number of New Zealanders killed in four and a half years of the brutal trench warfare that was even then raging in Europe. The sudden appearance and rapid spread of the disease left a bewildered and grieving population asking how, in an age of scientific wonders, such a thing could happen.
Many blamed Niagara, and two of its passengers in particular: the country’s prime minister, William Massey, and his deputy, Joseph Ward, who were returning from War Cabinet and Imperial War Conference meetings in London.
The steamer’s captain had radioed for assistance as the vessel, fresh from Vancouver, Canada, via San Francisco, Hawaii and Suva, approached the New Zealand coast. There were, he said, 100 cases of the deadly Spanish flu among the 567 passengers and crew. The bosun’s mate was dead and 25 people were in need of urgent hospital treatment.
Health authorities knew what might be in store. In early July, the highly infectious new strain of influenza had swept through the Western Front, felling soldiers and civilians alike. A second wave, even more virulent than the first, soon followed, and—unusually for influenza it struck the Southern hemisphere even as it rampaged unchecked in northern cities. By October, the flu was at its height in countries as far apart as South Africa, China, Japan, Peru and Italy.

New Zealanders had had their first taste of the contagion six weeks earlier when England-bound soldiers of the 40th Reinforcement, aboard the transport Tahiti later dubbed the “death ship”—called at Sierra Leone. Although no one left the vessel, the troops contracted influenza from infected locals loading coal. Within days, half of all those on board, including all the doctors and most of the nurses, were ill. More than 80 died.
By the time Niagara neared the dock in Auckland on October 12, its own sick list had swollen to 130. Nevertheless, after some hesitation, local health authorities cleared the ship, Massey and Ward went about their business and the unwell were carried to hospital. Within a week, three of the ship’s patients—two crew and a nurse—were dead. Soon, people unconnected with Niagara were falling ill, struck down with nausea, coughing, headaches, aching bodies and high temperatures. Many developed pneumonia, their skin taking on a blackish hue as lung damage choked the supply of oxygen to the blood and caused blood vessels throughout the body to rupture.
As the virulent disease caught hold, life in the city began to unravel—three-quarters of Auckland Hospital’s nurses fell ill, telephones worked only three hours a day for lack of operators and fire stations were all but deserted. The flow of people and goods slowed as hundreds of railway employees lay sick, as did many of the city’s watersiders and tram workers. Schools were turned into makeshift hospitals. Billiard halls, cinemas, classrooms and hairdressers were shut. Race meetings, church services and even funeral gatherings were banned and—such was the death toll—delivery vans were requisitioned as hearses.
Such scenes were repeated in other towns and cities as the influenza spread, while the Public Health Department, unused to epidemics and with no effective weapons at its disposal, resorted to bland messages of good cheer and the dispensing of zinc sulphate vapours.
The pandemic reached its height in late November at one point more than a thousand bodies lay in Auckland’s Victoria Park, awaiting funeral trains to the city’s Waikumete Cemetery. But by December, the worst was over. Outbreaks became fewer, patients recovered and the country began to nurse its wounds.
The influenza, which came as a thief in the night and lashed the land with irresistible fury, vanished as suddenly and inexplicably as the plagues of old.
A commission of inquiry set up to answer public criticism of the government’s response to the epidemic found that it had been introduced from outside the country and that “there is a strong presumption that the clearing of the ship Niagara was the cause”.
The verdict, which confirmed popular opinion at the time, now appears unjust. It is true that Massey, the leader of the ruling Reform Party and a staunch imperialist, had little time for Ward, the leader of the opposition and a Catholic to boot, whom fate had thrown onto the government benches. After many weeks together in Europe, and following the long confinement of a sea voyage, any delay in disembarking would have been irksome to both men. Nevertheless, it is doubtful that political strings were pulled. When infection struck on Niagara, Massey had insisted that he and Ward have no special treatment—the prime minister had even lent a hand running the ship’s dining room.
Doctors sent to investigate the outbreak aboard Niagara had reported that it appeared to be the common influenza that every year made its appearance in New Zealand. Indeed, six people had died of flu shortly before Niagara arrived. Moreover, several other vessels which had sailed from Northern hemisphere ports—some carrying invalided soldiers from the front—had berthed unexamined and unhindered earlier in the month.

If the haste with which Niagara was cleared revealed health officials’ reluctance to inconvenience their political masters—Fiji had no such qualms about refusing to allow Niagara to dock—it was also a sign of how the country’s long isolation had left it unprepared for what announced itself as the scourge of the new century—viral attack.
Even the way viruses worked took some getting used to. It was well known that natural selection shapes all living things. The more organisms there are, the more natural variations can occur. The simpler their form, the more radical the possible variants. And the faster the life-cycle, the more variants are possible in a given period. But rather than billions of individual organisms struggling to propagate, viruses, the smallest, most abundant organisms on Earth, seemed to behave almost as a single organism, constantly testing human defences, shape-shifting and weaving through the population with a kind of determination and intelligence.
The grim total of New Zealand’s Spanish flu victims, which in some stricken communities reached 45 dead for every thousand inhabitants, nevertheless seems modest in the context of the staggering global devastation. In the course of just a few months the virus killed between 50 and 70 million people on six continents—three percent of the world’s population—and left almost no community untouched. It was a cataclysm of biblical proportions and it sent epidemiologists scouring ancient plague records for adequate comparisons.
[Chapter Break]
If New Zealand’s experience of the 1918 influenza pandemic can be said to have had an upside, it was this: it triggered the passing, soon after, of a new Health Act claimed by many as the best of its kind in the English-speaking world.
Lance Jennings, a clinical virologist with the Christchurch School of Medicine and Health Sciences and one of the world’s leading influenza specialists, traces the origin of the country’s public health service to the 1918 influenza outbreak. It was a growing concern at the likelihood of another such pandemic—and a realisation that neither the World Health Organization nor individual governments were taking the prospect seriously—that, in 1996, prompted Jennings to sketch out a contingency plan.
“I still have the envelope I drew it up on,” he told me.
Jennings then found himself charged with formalising New Zealand’s influenza-control and pandemic-preparedness strategies, which were among the first in the world. In 2002, the country again took the lead, becoming the first to hold a national pandemic readiness exercise.
It was to be no token gesture. Jennings’ plan became a blueprint for the national response to the outbreak of SARS (severe acute respiratory syndrome), which flared up in China’s Guangdong province in November 2002 and, thanks to modern air networks, rapidly spread to 37 countries before being contained. The death rate among the more than 8000 people infected by the SARS corona-virus approached 10 per cent.
Equally worrying was another viral outbreak that had started when the highly pathogenic H5N1 bird flu virus leaped directly from poultry to humans. That was in 1996, the year Jennings scribbled those notes on his envelope. On that occasion, ground zero was Hong Kong, and the avian virus killed six of the 18 people it infected before a massive bird cull choked it off.
Between 2003 and October 2007, H5N1 proved itself even more lethal, killing 201 of the 329 people it infected. To seasoned virologists a 60 per cent mortality rate sounds loud alarm bells. What would happen if such a lethal virus, having once crossed from bird to human, learned to jump between humans as easily as seasonal influenza does?
The world has witnessed the emergence of a string of novel influenza strains since 1918, including two more pandemics, Asian flu in 1957–58 and Hong Kong flu in 1968–69. Nor were birds the only source of inter-species viral infection. In 1976, four soldiers at a United States army base in New Jersey caught swine flu. One died.
When, in April 2009, Mexico reported H1N1 swine flu fatalities in its population, the nightmare scenario resur faced of a lethal, unstoppable human virus. Within weeks, human infections were confirmed in the neighbouring United States and soon afterwards in other countries as well. By late June, someone at the Atlanta-based Centers for Disease Control and Prevention (CDC) used computer modelling to extrapolate reported cases and claimed that the United States had “at least” a million cases of swine flu—the majority among young people.

Long before then, New Zealand’s health authorities were fighting H1N1 on home ground. On April 25, a group of students and teachers from Rangitoto College on Auckland’s North Shore were quarantined upon their return from a study trip to Mexico when they began to show flu symptoms. Several were later admitted to hospital and all were treated with the antiviral drug Tamiflu, along with their immediate contacts. A returning party from nearby Northcote College was also isolated, and swab samples from both groups, identified as likely to be H1N1 influenza, were sent for confirmation to the World Health Organization Collaborating Centre for Influenza (WHOCC) in Melbourne. On April 28, as the death toll from swine flu in Mexico approached 150, Melbourne confirmed that three Rangitoto students had tested positive for H1N1 and that others were likely to have contracted it. The Northcote College group was cleared of infection.
The country was in the Ministry of Health’s “containment phase”—identifying potentially infected travellers, tracking down anyone they had come into contact with, swabbing individuals and treating confirmed cases with antivirals. This work fell on Auckland City Hospital, Canterbury Health Labs and the National Influenza Centre (NIC) at Wallaceville in Upper Hutt. Part of the WHO international network, the NIC was responsible for monitoring seasonal influenza and reporting any new viral strains so that flu vaccines could be updated. It was equipped with one of the country’s most advanced diagnostic laboratories for handling contagious disease, but as the number of suspected swine flu cases increased, the cumbersome goggles, double gloves and the long, involved procedures took their toll on staff. Sequencing of the genetic material took a minimum of 30 hours for each sample, and technicians worked around the clock to keep up with the stream of swabs.
A new diagnostic toolkit, developed by another WHO reference lab in Atlanta, Georgia, was rushed out to influenza centres around the world. It helped, but the need to handle the infectious samples with care caused bottlenecks.
The sense of emergency was heightened on June 11 when, after an emergency meeting, the WHO declared H1N1 an “unstoppable” global pandemic—the first of the 21st century. Since its appearance in April, the virus had spread to 74 countries, and in raising its alert to level six, the organisation said it was signalling geographic spread rather than an increased mortality rate.
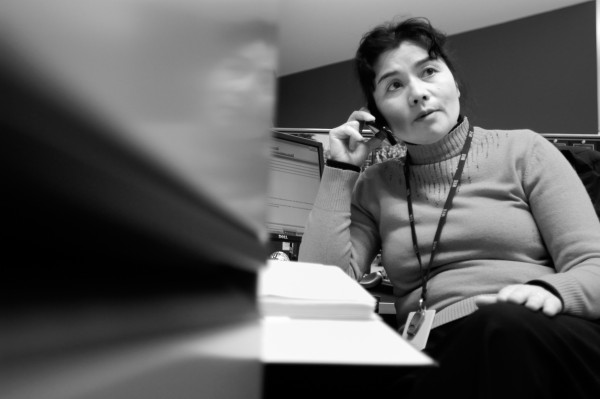
“I remember the week beginning 13 June,” says the NIC’s director, virologist Sue Huang. “We processed 1100 samples. It was at the limit of what we could manage, even with the help of MAF’s animal influenza reference lab and others.”
Unexpectedly, the punishing workload lightened the very next week. On June 22, the Ministry of Health announced that it had entered the management phase of its pandemic plan. Confirmed cases of swine flu had begun appearing among people with no clear connection to travellers, indicating that the virus had become established in the community. The sampling priority therefore switched to diagnosing and treating people most at risk. Others with suspected swine flu were told to stay at home until they had recovered, to limit the spread of infection.
“Containment worked in New Zealand,” says Huang. “It delayed the virus for seven weeks, which was a remarkable achievement.”
The delay was important for several reasons. It reduced the strain on hospitals and doctors as the country entered its regular flu season, and it bought time for the development of an effective H1N1 vaccine. Epidemiologists calculated that up to 60 per cent of New Zealanders would eventually become infected with swine flu and the long work of developing a vaccine and putting it through rigorous clinical trials would not be done before September at the earliest. Even seasonal inoculations took five months to get to market.
Once swine flu became established in Australia, there was little that could be done to stop it spreading here,given that seven airports link the two countries, says Huang. It is an issue that Jennings has wrestled with. Theoretically, the fact that New Zealand is an island nation makes the job of safeguarding it straightforward, but the economic necessity of maintaining the flow of trade and, significantly, tourists makes it highly problematic. Public health announcements on inbound flights help to raise awareness, as would the introduction of thermal imaging machines, says Jennings, although neither would stop someone determined to evade testing.
In any case, the political will is not there to close borders. Jennings learned that lesson when the Ministry of Tourism opposed several measures to reduce the risk from SARS. “The country’s economic security is more important than its public health,” says Jennings, “but we keep plugging away.”
Attending to borders is one of the standout lessons of 1918, a lesson learned hardest in Samoa, where in early November 1918 the island trader Talune arrived in Apia from Auckland, where it had tied up alongside Niagara. Talune’s prior landfall in Fiji had been blocked—sickness had broken out among the crew—but New Zealand-administered Apia was less vigilant. Crew were allowed ashore and within a week influenza was ravaging the main island, Upolu. It then crossed to nearby Savai’i. By the time it had run its course, 8500 people—a quarter of Western Samoa’s population—lay dead. Western Samoa suffered the world’s highest national death rate from the pandemic. Neighbouring American Samoa, by contrast, avoided the deadly flu entirely by imposing a total blockade.
[Chapter Break]
Frightening and unpredictable though they are, history suggests that, if anything, the tempo of globe-circling pandemics is picking up.
The archetypal pandemic is bubonic plague, a disease carried by rodents and transmitted to humans by fleas. Known as the Black Death for the discoloration due to massive haemorrhaging and high mortality rate, it first made its mark in the sixth century when it laid low Constantinople, the heart of the Byzantine Empire, and went on to kill a quarter of the population of southern Europe.
The next plague was probably picked up in China’s Yunnan province by Mongol horsemen who carried it to the fringe of Europe in the 14th century. returning genoese colonists then dispersed the infection throughout Europe and by 1348 a new pandemic had begun. In a relatively brief time it killed almost 30 per cent of Europe’s population. What is interesting about this second plague is the way it utterly transformed Western civilisation. There were the usual outbursts of hedonism, of course, and other signs of moral breakdown. A long-lasting fascination with death and the macabre was also evident in the arts. More importantly, the Church and the aristocracy emerged with less power, while widespread labour shortages improved the lot of the working class. With higher production costs and fewer people to buy goods, economic activity declined—the famous businesses of the Medicis in 15th-century Florence were notably smaller than the city’s biggest banking and commercial firms of 100 years earlier.
Micro-organisms are small, however, and with the passing of years easily overlooked. The student of history will search in vain for traces of Yersinia pestis, the bringer of the Black Death, in the work of the celebrated 19th-century historian Jacob Burckhardt. His seminal The Civilisation of the Renaissance in Italy fails to mention the plague anywhere in its 462 tightly packed pages. Even the 1918 Spanish flu, for all the misery it caused, was soon forgotten. Only now as pandemics reassert themselves despite all the artifice of our science and technology, are historians beginning to acknowledge the profound impact of these minute invaders.

Germ theory helped to take the edge off the third plague wave, which began in the 1850s, also in Yunnan, China. By 1896 it had reached India, where it killed some six million people, and triggered outbreaks in Thailand, Burma, Tunisia and Hawaii. The idea that such diseases were caused by living organisms and not by some miasma or “poisonous air”, as was once thought, led to more effective prevention. It helped that Y. pestis, the cause of bubonic plague, was a bacterium and therefore could be seen through a microscope.
Viruses, responsible for a long list of killer diseases including yellow fever, polio, measles, rabies, HIV, dengue and influenza, were more elusive. A hundred times smaller than bacteria—just 10–300 millionths of a millimetre in diameter—they were invisible under even the most powerful microscope. As late as 1902, The Century Dictionary, Cyclopedia and Atlas described viruses as a “morbid poison” produced in the body by a person suffering from a contagious disease and capable of “exciting” the same disease in others through inoculation. The same authority pinned down influenza as “an epidemic catarrh”. The word influenza itself derived from the Italian for “influence”, noted the Century Dictionary, and was so called because it was “supposed to be due to some peculiar atmospheric influence”.
It took the development of the ultraviolet microscope in 1925, and later of the electron microscope, to reveal viruses for what they really were. But how they functioned, even how they spread, was harder to discover. Early attempts to isolate the yellow fever “germ” that was laying waste to panama Canal labourers failed due to the small size of the agent responsible. Its eventual identification as a virus led to the first vaccine of the 20th century. Success against smallpox was more spectacular. In 1966, with 10–15 million people a year in 33 countries becoming infected, the WHO launched a decade-long eradication programme. Today, the world is free of the smallpox virus which, officially at least, exists in only two research laboratories—one in the United States and the other in Russia.
But, then, the Variola virus responsible for smallpox was a comparatively straightforward target. It did not infect ani- mals, and so had no place to hide or bide its time, it was easily diagnosed and a highly effective vaccine was available.
Influenza is another matter. Like all viruses, those causing human flu are intracellular parasites—little more than protein-coated packets of genetic code built from DNA or RNA and designed to penetrate and reprogramme host cells. Essentially, they take over the factory and retool it to make copies of themselves, often, but not always, destroying the original cell in the process. They have no ability to move independently but are able to remain dormant for long periods and can even be crystallised.
Because they consist of sets of instructions embedded in just eight gene segments, flu viruses are easily able to alter their behaviour by accumulating mutations in their genetic code—a process known as antigenic drift. Dr Huang’s National Influenza Centre, and others like it around the world, track this drift in order to create new seasonal vaccines.
More radical is the tendency among one of the three main groups of flu virus, Type A, to exchange genes. This process, known as antigenic shift, or reassortment, can create novel and deadly strains of human influenza. All the devastating flu pandemics, from 1918 on, have either been viral introductions or reassortments of Type A viruses.
What makes Type A influenzas both frightening and unpredictable is that, though their natural ecology is in aquatic avian species, they can infect a range of hosts, including birds and mammals. If a Type A influenza finds itself reprogramming cells in the same body as, say, a human influenza strain, the probability of antigenic shift is high. If that happens, the result could be a biological super weapon, one that combines the qualities of the two original strains, being both readily transmitted between humans and, because it is novel and therefore more easily able to bypass host immune systems, potentially lethal.
This was precisely what went through the minds of virologists in 1997 when an avian flu managed to cross what was thought to be an unbridgeable divide and infect a three-year-old boy in Hong Kong. United States-based New Zealander Robert Webster, a world authority on avian viruses and the person who had discovered that all avian flu originated in aquatic birds, confessed to having gone into “a state of panic” at the news. Previously, it was assumed that avian viruses first needed to make the leap to pigs before infecting humans. Yet here was an H5N1 strain that, having killed more than 70 per cent of the poultry on three farms, made straight for a child. Worse, a human strain, Sydney flu, had just arrived in Hong Kong and it brought with it information needed by the avian virus to move among humans. Only the large-scale butchering of birds—some two million in total—forestalled the possibility of an information-sharing episode.
Further human infection by new strains of the H5N1 bird flu in 2003 and 2004 underscored how likely antigenic shift was becoming. Sustained culls once again checked their spread but epidemiologists warned that one deadly strain was becoming endemic in Asia. Reports began to circulate that mutations had been detected in the flu carried by birds in Africa and Europe that made it more able to infect humans and to survive in the upper respiratory tract. Birds typically have a body temperature of 41º C, whereas humans have a normal temperature of 37º C, and noses and throats, where viruses usually enter, are even cooler. The ability to get a foothold in the upper respiratory system of mammals is important because it would give a virus the ability to infect a greater range of cell types and to spread more readily through coughs and sneezes. Researchers admitted that other mutations would also be needed before avian influenza became a human pandemic. Nevertheless, all that was needed, they implied, were sufficient rolls of the genetic dice. The 1918 pandemic is thought to have started out from bird flu in just that way.
[sidebar-1]
It was while all eyes were on the increasingly lethal avian influenza that the novel 2009 swine flu (H1N1) came out of left field. The influenza A virus took the world by storm and within weeks it had become a pandemic. A study of New Zealand swine flu cases in the first two weeks of June by researchers at the University of Otago, Wellington, and Utrecht University in the Netherlands indicated that it was more infectious than either seasonal flu or the 1918 Spanish flu. Initial estimates put the transmission rate at about 1.5, meaning that every two people sick with the virus would infect three others. The researchers found that the actual rate was closer to 1.96, suggesting that about 80 per cent of New Zealanders would contract the virus
The new data came in the wake of disturbing findings by an international team led by virologist Yoshihiro Kawaoka at the University of Wisconsin-Madison that showed that the H1N1 flu was more dangerous than suspected. Unlike seasonal flu, the new pathogen had the ability to infect cells deep in the lungs, causing pneumonia. This ability, said Kawaoka, was also evident in the virulent 1918 Spanish flu.
He added that, again like the Spanish flu, the virus could circle the world in increasingly lethal waves, becoming more pathogenic as it evolved over the Southern hemisphere winter and returned for the northern flu season.
Meanwhile, Dr Huang’s NIC team had noted a new characteristic of the H1N1 virus—its dominance over seasonal flu. Within weeks of its arrival in New Zealand, swine flu went from causing 10 per cent of flu infections to 80 per cent. Fortunately, said Huang, it could be controlled by the antiviral drug Tamiflu which, until a vaccine arrived, was the first line of defence. Seasonal flu, on the other hand, was almost completely resistant to Tamiflu.
In early July, the country had a total of 1195 confirmed infections, including its first swine flu-related deaths—two men and a young girl—and 11 others in intensive care. Despite a record number of seasonal flu immunisations, with more than 800,000 doses distributed nationwide by mid-May, Auckland medical centres were nevertheless reporting a flood of flu cases. White Cross clinics in the region were examining 3500 patients a day, a thousand more than normal, mostly as a result of swine flu.
Would swine flu mimic the 1918 epidemic? Like everyone, Huang was unsure. She hoped not. “But Australia has a lot of people on oxygenation in intensive care. And many of them are healthy, with no underlying conditions.”
[Chapter Break]
Interestingly, kawaoka’s research found that the greatest resistance to H1N1 was to be found in those, now in advanced old age, who had been exposed to the 1918 flu. This was further confirmation of the theory that the 1918 human, swine H1N1 and 1979 H1N1 influenza A viruses were all recently descended from avian influenza A genes, and that some had found their way to the pandemic human H1N1 strain (see diagram). Researchers from the US National Institutes of Health went further, saying that the tenacious Spanish flu of 1918, the most mobile and lethal pandemic the world has ever seen, had founded “a viral dynasty” that persisted to this day “by drawing on a bag of evolutionary tricks to survive in one form or another”.
What makes influenza viruses so hard for immune systems to get the measure of comes down to changes in two of their eight genes. Hemagglutinin (H) and neuraminidase (N) code for surface proteins that enable the virus to enter a host cell. There are 16 H subtypes and 9N subtypes, resulting in 144 possible HN combinations. So far only three (H1N1, H2N2 and H3N2) have been found in viruses that are good at spreading among humans. But changes in these genes, along with alterations, large and small, elsewhere within the virus make it hard for host antibodies to recognise the invaders.

For almost a century, it seems, human immune systems have been locked in a complicated cellular dance with the progeny of the 1918 virus for control of the human body. The dance floor, if this analogy is to hold good, must broaden to include the planet’s vast bird population which, to viruses, is a global avian reservoir. Writing in the New England Journal of Medicine, researchers David Morens, Jeffery Taubenberger and Anthony Fauci explained that within this reservoir, avian flu viruses are stably adapted to the intestinal tracts of hundreds of bird species, and individual birds are often infected by several strains, resulting in prolific gene reassortment. “Because of this continual reassortment, a seemingly endless variety of new viruses with potentially new properties are continually being engineered. Indeed, thousands of unique gene constellations making up avian influenza viruses have already been identified.”
The long-term forecast: more of the same.
Viruses are emerging from the shadows to haunt us at an accelerating rate—not only influenza, but evolving insect-borne diseases that are spreading from the hothouse laboratories of the tropics as global warming opens virtual land bridges to new parts of the globe. Genetic studies suggest that some 80 per cent of infectious diseases arise in the tropics, and researchers at Australia’s James Cook University claim to have found evidence that tropical climates have already shifted more than six degrees of latitude beyond their former boundaries.
It is tempting to picture viruses as ruthless assassins, determined to kill at all costs, but Jennings for one doesn’t think that a helpful exercise. “A pathogen would not be very successful if it killed everyone,” he says.
“Viruses are better genetic engineers than us—they adapt to the population they move in.”
And it is useful to remember that most of those who died in 1918 were killed by bacterial pneumonia, a by-product of viral infection. Which is not to say viruses don’t have blood on their hands.
It could be, as my son quipped, that essentially they are colds that have got out of hand and are making mistakes. But who would be willing to risk lives—perhaps millions of lives—by gambling on these minute, opportunist gene gangs eventually getting it right. That would not be human nature. The viral trench warfare that began so spectacularly in 1918 is set to continue for, as a virologist might say, “as long as it takes”.