Brains, blood and British beef
AIDS, Hepatitis B, Ebola—new health hazards spring up on every side. Now it seems possible that mad cow disease, itself only a decade old, is spreading to humans.
On March 20, 1996, the British Ministry of Health triggered domestic turmoil and international panic when it announced that the hitherto obscure Spongiform Encephalopathy Advisory Committee had reported 10 recent and unusual cases of Creutzfeldt-Jakob disease (CJD), a rare degenerative condition, invariably fatal, that normally affects humans of middle age or older.
What was alarming about the 10 cases was their relative youthfulness—in persons aged 19-41, with a mean age of 29. Of 185 cases of CJD diagnosed in the UK since May 1990, the mean age at onset was 65 years. Only two cases younger than 45 had been seen, and they were both in 44-year-olds. Going back to 1970, there had been only a single case in a person younger than 30 years of age.
Symptoms and brain pathology of the 10 unusual cases were all similar and somewhat different from normal CJD. The most likely explanation for these cases, the committee concluded, was that the affected people had been exposed to bovine spongiform encephalopathy (BSE), popularly known as mad cow disease. While the cases did not prove any link between BSE and CJD, the committee noted that they were “cause for great concern.”
Those few words brought to a sudden end 10 years of assurances that eating British beef could never pass BSE to consumers, and plunged the British beef industry into chaos.
Overnight, CJD were the initials on everyone’s lips. Farmers in New Zealand were alarmed (not for the first time) about the possibility of BSE spreading to our cattle through the importation of semen and embryos from Britain. Within weeks the government banned such imports.
Then, in early May, CJD made local headlines again. At least one person who had recently died from the disease was found to have regularly donated blood in this country, some of which had been used to make blood products. Should the batch be discarded? Was it safe? Should recipients of such products be notified?
So far, only fragments of the CJD story have gained much currency, yet only by understanding the background of CJD and its possible links with BSE and other diseases can these questions of public health be satisfactorily answered.
CJD is one of a group of human and animal diseases thought to have similar causes. Scrapie, a disease of sheep and occasionally of goats, is the most studied and “senior” member of the group.
Scrapie is widespread in Europe, Asia, and America. Affected animals display a lack of coordination in their movements (ataxia), wasting and often severe itching of the skin, causing the animals to rub, and giving rise to the name scrapie.
It is not clear how the disease is transmitted. Infected ewes can pass it on to their lambs, although not usually in utero, but older sheep pick it up only after prolonged contact with infected animals. The disease can also be caught from land on which scrapieinfected sheep have grazed.
It often takes many years for infected animals to show symptoms, and we may be certain that many latently infected animals have been slaughtered and eaten over the years. There is no record of scrapie having been transferred to humans from sheep.
Scrapie is absent from New Zealand sheep and goats. In fact, after sheep imported during the 1970s had been in quarantine several years, first at Mana Island, then on a block near Rotorua, scrapie did appear amongst them. The whole consignment was destroyed and the two areas where they had been held were proscribed forever from having sheep graze them. Such is the seriousness with which the disease is held.
As most people have now heard, BSE is considered to have arisen during the late 1970s when sheep meal from scrapie-infected sheep was incorporated into cattle feeds. Since 1986, more than 150,000 cattle have died of BSE in Britain, and 31,000 farms have been affected.
Diseases similar to BSE have also been found in recent years in farmed minks, domestic cats, captive wild cats (puma, cheetah, ocelot), and captive wild ruminants (nyala, gemsbok, eland, Arabian oryx, greater kudu, scimitar-horned oryx), presumably all contracted through contaminated feed.
Experimental injection of brain extracts from BSE-infected cattle have transferred the disease to mice, cattle, sheep, pigs and, recently, a marmoset monkey.
All these animal diseases share certain features. Ataxia, behavioural changes and a lengthy period (up to a decade) between exposure to the infectious agent and manifestation of symptoms are common to all. Examination of the brains of infected animals shows extensive degenerative changes—clumps of fibrous material (plaques), and small holes that give the brain a spongelike appearance under the microscope (hence the name spongiform encephalopathies) are common (see photograph).
In 1921, the German psychiatrist Alfons Jakob described a disease of middle to late adult human life which he termed spastic pseudosclerosis, characterised by abnormalities of behaviour and intellect, weakness, spasticity, ataxia, rigidity, slowness of movement, tremors and hesitant speech. His countryman Hans Creutzfeldt had earlier identified a degenerative, possibly familial disease that was not too different, and in 1922 the two diseases were lumped together as CJD.
Between 1921 and 1968, only 150 cases of CJD were reported in the medical literature. Incidence has since been estimated at about one case per million people per year worldwide, although in a few groups it is much higher. Amongst Libyan Jews for instance, there are up to 75 cases per million per year. At one stage this high incidence was attributed to the local custom of eating lightly cooked sheep’s brains and eyes, but scrapie is very rare amongst North African sheep, and the idea has been discounted.
Ten to 15 percent of all cases of CJD occur in family groups, but the rest are sporadic cases. Age of onset is typically 60-65 and there are few cases in people over 80 or under 50. The disease is invariably fatal, death occurring within four to twelve months of the onset of symptoms.
Two American medical anthropologists, Gajdusek and Zigas, described another disease in 1957 that proved to be related to CJD, although its circumstances were very different. “Kuru,” as it is known, occurred at high frequency (one percent of the population per year) among the 35,000-strong remote Fore people of New Guinea. All age groups were susceptible, but the disease was less common among adult men than women.
In the Fore language kuru means shivering, and this disease was characterised by ataxia and tremor that progressed to complete physical incapacity and death in less than a year. The disease was spread by ritual cannibalism. As a rite of mourning and respect for dead kinsmen, the brain case was opened and the brain, along with other flesh, lightly cooked and eaten. Children and women were the main mourners.
Transmission could have been through eating brain (by far the most infectious tissue in the body), or wiping infectious material into abrasions, rubbing eyes, picking noses and the like. Washing was almost unknown among these people.
It has been suggested that kuru arose from a sporadic case of CJD that became an epidemic in the distinctive cultural context of the New Guinea highlands. With the cessation of cannibalism, the disease has largely disappeared.
Even more recently, another human disease akin to CJD and kuru has been discovered—fatal familial insomnia (FFI). Untreatable insomnia progresses to impairment of the autonomic and motor systems, and in advanced cases complex hallucinations arise followed by stupor, coma and death. Mean age of Onset is 49, and the disease runs its course in about a year.
The jaw breaking Gerstmann-Straussler-Scheinker disease (GSS) is the final human disease in the group. It, like FFI, is inherited, and some 50 extended families have been found with it. A loss of coordination precedes dementia, and death can take up to six years.
[chapter-break]
What causes this group of animal and human diseases is a puzzle. The great majority of infectious diseases are caused by microbes—protozoans, fungi, bacteria and viruses, all minute but containing the essentials of life: nucleic acids and proteins.
Identifying the infectious agent that caused scrapie proved a problem from the start. It was resistant to ultraviolet radiation, radioactivity, heat, formaldehyde, and enzymes that destroy most proteins and nucleic acids—collectively, agents that kill all life forms known.
In brain extracts that were highly infectious, electron microscopy could detect no virus particles. Furthermore, there was not a smidgen of evidence that the host’s immune system was even slightly excited by its owner’s slow demise—almost unheard of in an infectious disease. For a long time biologists regarded the elusive agent as an unconventional slow acting virus, and some still do.
Then a heretic or two suggested that since no sign of nucleic acid could be detected, maybe the infectious agent lacked both DNA and RNA. This is as fundamentally radical an idea as having a volcano without heat, smoke without fire, motor racing without wheels.
Stanley Prusiner, a professor at the University of California in San Francisco, has been the main proponent of the idea, and he is no longer being regarded as a flat-earther. He has christened the infectious agents that underlie all these diseases “prions,” and obtained strong evidence that the infectious agent is an altered form of a single protein, which he has called PrP (for Prion Protein).
In normal animals, PrP is a regular protein coded for by an everyday gene made of DNA, and is best known on the surface of brain cells. In studies reported only a few months ago, mice have been genetically engineered which lack PrP entirely. They develop, reproduce, and learn normally, but show marked disturbance of sleep and daily patterns of activity— an interesting reflection of FFI.
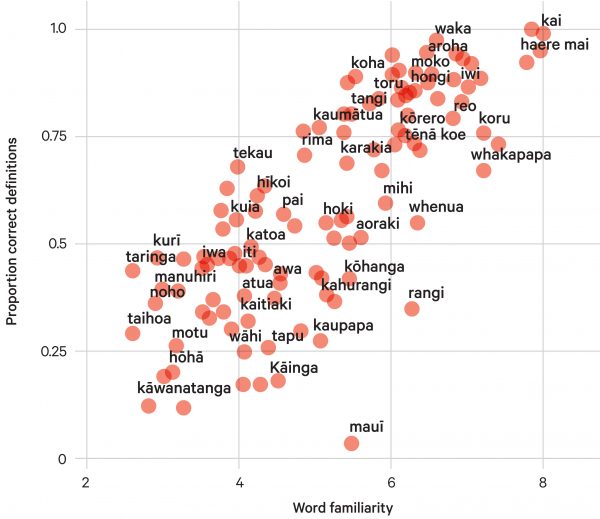
As with all proteins, PrP is folded in its own unique and characteristic way—something like two parallel coil springs resting on top of two more springs that point off at an angle towards top left (see figure).
In patients with spongiform encephalopathies, the conformation of the PrP protein is altered so that the top two coils unravel to form a sheet-like structure. The altered structure of this one protein alone seems to gradually lead to the formation of plaques and holes in the brain that eventually produce dementia and death.
In the spongiform encephalopathies passed genetically from one generation to the next in familial groups, subtle mutations in the DNA that codes for the PrP protein underlie the changed shape. However, simple genetic diseases such as cystic fibrosis or Huntingdon’s disease are never infectious, whereas GSS, FFI and familial CJD have all been experimentally transmitted to animals.
Kuru, scrapie, and BSE are clearly infectious. In sporadic CJD, scrapie and BSE, there do not seem to be mutations in the PrP gene, but nonetheless much of the PrP exists with an altered conformation, termed PrPs’ (Sc for scrapie). The protein seems to have spontaneously changed its shape. This altered PrPs’ protein is apparently infectious in its own right, quite apart from DNA.
According to the prion model, when PrPs’ protein molecules are introduced into a new host, they act as templates that cause the host’s normal PrP proteins to adopt the altered conformation. A domino effect is thought to take place, so that host PrP altered to PrPs’ then acts as template for more host PrP to convert, and as more and more host PrP takes on the PrPs’ conformation, disease starts to take hold.
So these are diseases that can be acquired in several ways. In the inherited version, a mutated gene is responsible for passing on the illness; in the infectious form, disease is transmitted by the altered protein itself. In sporadic CJD, nobody knows what triggers the formation of PrPs”.
Surprisingly, quite a body of sophisticated evidence supports this strange scenario, which to anyone possessing a modicum of biology would at first glance (and second and third) seem to rest more comfortably in Hollywood than Harvard.
As noted earlier, scrapie does not seem to be transmitted to humans, although it can infect other species. Transmission of prion disease across a species barrier seems to be difficult, although the difficulty is more readily surmounted in closely related species. The issue seems to be how similar the PrP molecules are between the two species. If they are similar, transmission is easier.
Sheep and bovine PrP differ at seven amino acids out of 254 that make up the protein, whereas human and bovine PrP differ at more than 30 positions. This should mean that the likelihood of BSE crossing into humans is low. However, with the number of exposed Britons estimated at 50 million, even improbable events can occur.
Experiments in which the gene for human PrP has been inserted into mice (and both human and mouse PrP protein produced), then BSE PrPs’ introduced have so far resulted in the conversion of only mouse PrP to PrPs’, but the experiment should run for another two years before it is conclusive.
(It should be noted that in these experiments the transgenic mice have been challenged with BSE by intracerebral inoculation, a route that in mice is 100,000 times more efficient at causing infection than oral exposure.)
Before the advent of BSE, few people were exposed to PrPs’. Some 100 cases of CJD occurred iatrogenically (accidental spread through a medical procedure). These included corneal transplantation, implantation of contaminated EEG electrodes, neurosurgical procedures and transplantation of tissues.
The accidents are understandable. The resistance of PrPs’ to most sterilising agents renders disinfection of operating theatres extremely difficult. Any surgery patient could be asymptomatically afflicted by CJD given its long incubation time.
But by far the major cause of iatrogenic infection has been treatment with human growth hormone preparations (made from pooled human pituitary glands taken from brains of cadavers at autopsy) between the late 1950s and 1985. Worldwide, about 80 cases have so far developed from some 16,000 recipients of growth hormone. In New Zealand there have been five cases of CJD among 174 treated with growth hormone. (A total of 41 people have died from CJD in New Zealand between 1980 and 1995.)
Of broader concern is the possibility of transmission of CJD through blood and blood products such as factors VIII and IX, prepared for haemophiliacs. Blood products are made from “pools” of donated blood to which 10,00015,000 donors contribute.
CJD is thought to have an incubation period of up to 30 years before symptoms appear, and unknowingly afflicted persons can innocently donate blood during this interval. Is such blood, or products made from it infectious?
Though PrP (and PrPs`) is most abundant on the surface of cells in the central nervous system, small amounts occur on the surface of white blood cells, in eyes, tonsils, spleen and thymus. The amount present in blood fluid is probably very small.
Although blood transfusion has been practised much more widely and for a much longer time than growth hormone therapy, there is no evidence that CJD has been passed on by this route. Bear in mind that CJD is not a new disease. It has been around for much longer than blood transfusion. It would not be unreasonable to assume that most, if not all, blood products ever made from large pools of donated blood worldwide have been contaminated with CJD!
Despite this disconcerting possibility, rates of CJD among recipients of transfusions are identical with rates in control groups. No identified recipients of blood from donors who have later died from CJD have so far developed the disease, and none of more than 2000 CJD patients studied over the last 20 years worldwide has been shown to have acquired the disease from a donor who later died of CJD.
Nor have intensive users of blood products such as haemophiliacs been infected with CJD from preparations they have used. This is not to say that haemophiliacs don’t get CJD, just that they don’t get it any more frequently than anyone else.
Nevertheless, donations of blood from persons considered at risk for CJD (family history, growth hormone treatment, certain fertility treatments) are no longer being accepted.
While the possibility of blood-borne infection cannot be categorically excluded (can anything?), a reasonable body of evidence suggests that the possibility of such infection is vanishingly small.
Those who seek 100 per cent assurances that blood products are safe will never get them. Even without CJD, such assurances would not be given. Science works in probabilities, and the probability of getting CJD from blood products is very small. Nobody knows for sure how small, perhaps 1 in 10,000 or 1 in 100,000, but to a scientist there is a big distinction between such long odds and zero. Only vampires take blood products as a dietary supplement—others take them to stay alive. Without them their chance of death may be, say, 1 in 10 or 1 in 100 within five years.
BSE is not an issue locally, but for those of nervous disposition visiting the UK, bovine muscle tissue is thought to be safe to enjoy (it does not contain PrP), but more anonymous meat mixtures such as sausages would be more suspect. However, since 1989 “specified bovine offals” (brain, spinal cord, spleen, thymus, tonsils) have been legally banned from human and cattle foods in the UK, so mince and sausage should be OK.
But a niggle remains here. Although the incidence of BSE among cattle is declining, it is not falling anywhere near as rapidly as was predicted in 1989. A question mark hangs over how it is now being transmitted—if not through feed, and not from mother to calf, and not by animal to animal by contact, how are cases still arising in, say, four-year-old cows? One possibility is that BSE is still entering the food chain.
The heat resistance of PrPs’ means infectious particles are not destroyed by normal cooking, and they are also resistant to digestion by protein-digesting enzymes in the gut.
How PrPsc gets from gut to brain is mysterious, but, as BSE proves, the process clearly occurs in cattle and other species. Eschew bovine brains for a while yet.